Sphingobacterium spiritivorum что это
Первый корейский случай саркоидоза Sphingobacterium spiritivorum у пациента с острой миелоидной лейкемией
Sphingobacterium spiritivorum редко выделяется из клинических образцов пациентов с ослабленным иммунитетом, и до сих пор не было сообщений о случаях инфекции S. spiritivorum в Корее. Мы сообщаем случай бактериемии S. spiritivorum у 68-летней женщины, у которой был диагностирован острый миелоидный лейкоз, а затем получил химиотерапию. Через день после окончания химиотерапии температура тела увеличилась до 38,3 ℃. Грамотрицательная палочка была выделена в аэробных культурах крови и идентифицирована как S. spiritivorum с помощью автоматизированной биохимической системы. Анализ секвенирования 16S рРНК подтвердил, что изолятом является S. spiritivorum. Пациент получил антибиотикотерапию в течение 11 дней, но умер от септического шока. Это первый зарегистрированный случай заражения человека S. spiritivorum в Корее. Хотя человеческая инфекция встречается редко, S. spiritivorum может быть фатальным оппортунистическим возбудителем у пациентов с ослабленным иммунитетом.
Виды Sphingobacterium являются неферментирующими, грамотрицательными стержнями, которые являются положительными для биохимических испытаний, таких как производство каталазы и оксидазы, но являются отрицательными для индола [1]. Виды Sphingobacterium ранее были описаны как неназванные бактерии (часть Центров по контролю и профилактике заболеваний группы IIk). Holmes et al. [2, 3] предложил название рода Flavobacterium для бактерий, тогда как в 1983 году Yabuuchi et al. [4] впервые предложил название Sphingobacterium для рода. Род Sphingobacterium был создан для классификации организмов, которые содержат большое количество сфингофосфолипидных соединений в их клеточных мембранах, и имеют другие таксономические особенности, которые отличают их от видов Flavobacterium [4].
Виды Sphingobacterium обычно выделяются из почвы, растений, пищевых продуктов и источников воды, но изоляция видов от клинических образцов человека редко сообщается во всем мире [5]. Кроме того, Sphingobacterium spiritivorum редко выделялись из клинических образцов пациентов с ослабленным иммунитетом, и в нашей стране не было сообщений о случаях инфекции S. spiritivorum в Корее. Мы сообщаем случай бактериемии S. spiritivorum у пациента, прошедшего химиотерапию для острого миелоидного лейкоза.
68-летнюю женщину поместили в нашу больницу для одышки, которая длилась 7 дней. У нее не было истории о курении или легочных заболеваниях. Физическое обследование не выявило лимфаденопатии или органомегалии. Начальный полный подсчет клеток крови показал следующие результаты: гемоглобин, 11,3 г / дл; белых кровяных телец, 2,86 × 109 / л (нейтрофилы, 40%, лимфоциты, 57% и моноциты, 3%); количество тромбоцитов, 47 × 109 / л. Мазок периферической крови выявил панцитопению без лейкемических взрывов.
Для оценки панцитопении проводили обследование костного мозга (БМ). Магмы аспирации BM и цитохимическое окрашивание показали увеличение миелобластов (40%) и других миелоидных предшественников. Пациенту был поставлен диагноз острый миелоидный лейкоз, который не был определен иначе, в соответствии с классификационной системой ВОЗ 2008 года [6].
Она получала химиотерапию цитарабина 160 мг и идарубицина 20 мг в течение 3 дней и идаруцицина 20 мг в течение 4 дней. Через день после окончания химиотерапии температура ее тела увеличилась до 38,3 ℃. Ее кровяное давление, частота пульса и частота дыхания составляли 90/70 мм рт.ст., 110 / мин и 20 / мин соответственно. Уровень C-реактивного белка (CRP) увеличился до 6,31 мг / дл, а уровень прокальцитонина составил 0,08 нг / мл (контрольный диапазон: 99% с S. spiritivorum и> 0,8% от других видов. Таким образом, изолят был подтвержден как S. spiritivorum [7].
Для филогенетического анализа полученную последовательность сравнивали с результирующими штаммами наиболее близкородственных видов Sphingobacterium, присутствующих в базах данных GenBank. Филогенетическое дерево было построено методом соседнего соединения с использованием последовательностей Microseq 500 bp 16S рРНК (фиг.2).
Противомикробную восприимчивость тестировали с использованием карточки AST-N132 системы Vitek 2 (BioMérieux). Изолят восприимчив к цефепиму, ципрофлоксацину, левофлоксацину, меропенему, миноциклину и триметоприму сульфаметоксазолу; имели умеренную восприимчивость к цефотаксиму, цефтазидиму, имипенему и тикарциллин-клавулановой кислоте; но был устойчив к амикацину, азтреонаму, колистину, гентамицину, пиперациллину, пиперациллин-тазобактам, тикарциллину и тобрамицину.
Центральный венозный катетер был удален. Режим антибиотика был изменен с цефепима на ципрофлоксацин, поскольку подозревали, что нефротоксичность обусловлена увеличением уровня мочевины мочевины и уровня креатинина в крови. Через 3 дня лихорадка пациента стихла. Последующие тесты на культуру крови были отрицательными для S. spiritivorum и любого другого микроорганизма. Однако на пятый день терапии ципрофлоксацином у нее снова развилась лихорадка, и общее состояние ухудшилось. В одиннадцатый день она умерла от септического шока.
Сфингобактериальные виды обычно выделяются из почвы, воды и растительного материала, и только несколько сообщений о человеческих инфекциях, вызванных видами, опубликованы [5]. Ранее сообщаемые виды Sphingobacterium, выделенные из клинических образцов человека, были S. multivorum и S. spiritivorum. На сегодняшний день сообщалось о 7 случаях заражения S. multivorum по всему миру в связи с септицемией [5, 18-20], перитонитом [21], инфекцией дыхательных путей [22] и некротизирующим фасцитом [23]. Сообщалось только о 3 случаях инфекции S. spiritivorum во всем мире 24. Настоящий случай и ранее сообщенные случаи сравниваются в таблице 2. В 2002 году Маринелла [24] впервые описала случай сепсиса, связанного с целлюлитом, вызванного инфекцией S. spiritivorum. В 2003 году Tronel et al. [25] сообщал случай бактериемии S. spiritivorum. В 2005 году Kronel et al. [26] сообщил случай сепсиса, связанного с целлюлитом, вызванного S. spiritivorum из водоема парового утюга.
В данном случае пациент находился в состоянии иммуносупрессии из-за химиотерапии для лечения острого миелоидного лейкоза. Пациенту была поставлена диагноз связанная с катетером инфекция кровотока, потому что временной интервал положительных признаков культуры крови от периферической вены и центральных венозных катетерных культур составлял более 2 часов. Источником и способом передачи инфекции S. spiritivorum в этом случае могло быть место входа в кожу внутрисосудистого устройства или подкожный путь катетера, который находился в непосредственной близости от естественных мест обитания этого организма.
Анализ секвенирования 16S рРНК может быть полезным и окончательным методом, особенно для идентификации клинически значимых бактериальных изолятов с неоднозначными биохимическими профилями или редко встречающимися бактериальными видами [27, 28]. Мы подтвердили идентичность изолята крови, сначала идентифицированного биохимически как S. spiritivorum, путем анализа секвенирования 16S рРНК.
Виды Sphingobacterium, как правило, устойчивы к аминогликозидам и полимиксину B, но восприимчивы к хинолонам и триметоприму-сульфаметоксазолу in vitro. Известно, что чувствительность к β-лактамным антибиотикам изменяется [1]. В 2009 году Lambiase et al. [29] сообщили, что 13 штаммов S. multivorum и 8 S. spiritivorum из образцов мокроты у 332 пациентов с кистозным фиброзом были устойчивы к аминогликозидам, но восприимчивы к хинолонам и триметоприму сульфаметоксазолу. Они также обнаружили, что S. multivorum изоляты устойчивы ко всем β-лактамам, тогда как изоляты S. spiritivorum восприимчивы к цефтазидиму, пиперациллину и карбапенемам. Изолят этого случая был восприимчив к цефепиму, меропенему, миноциклину, а также к ципрофлоксацину, левофлоксацину и триметоприму сульфаметоксазолу.
Это первый зарегистрированный случай заражения человека S. spinivorum в Корее, который показывает, что S. spiritivorum может быть фатальным человеческим оппортунистическим возбудителем у пациентов с ослабленным иммунитетом, несмотря на то, что человеческая инфекция встречается редко.
Эта работа была поддержана двухгодичным исследовательским грантом Пусанского национального университета.
Не сообщалось о потенциальных конфликтах интересов, имеющих отношение к этой статье.
(A) грамотрицательные бациллы из препаратов мазка положительных культур крови (окраска грамма, × 1000). (B) Колонии желтого цвета Sphingobacterium spiritivorum на пластине из агара.
Филогенетические связи изолята от настоящего пациента и родственных видов Sphingobacterium, построенных методом соседнего соединения с использованием последовательностей 16S рРНК Microseq 500 bp. Все имена и номера доступа указаны в базе данных GenBank. Дерево было вытянуто с длиной ветвей как эволюционные расстояния. Длина шкалы 0,01 указывает на 1% последовательности.
Сравнение последовательностей изолята от пациента и его наиболее похожих видов
База данных: GenBank (http://www.ncbi.nlm.nih.gov/genbank), EMBL (Европейская лаборатория молекулярной биологии, http://www.ebi.ac.uk/embl), RDP-II (The Ribosomal Database Project, http://rdp.cme.msu.edu) и EzTaxon (http://www.eztaxon.org).
Случаи инфекции Sphingobacterium spiritivorum
Сокращения: M, мужчины; F, женщина; БАЛ, бронхоальвеолярный лаваж; PR, настоящий отчет; NA, недоступно.
Sphingobacterium spiritivorum bacteremia due to cellulitis in an elderly man with chronic obstructive pulmonary disease and congestive heart failure: a case report
Abstract
Background
Sphingobacterium spiritivorum is a glucose non-fermenting Gram-negative rod, formerly classified as one of the Flavobacterium species. It is characterized by a large number of cellular membrane sphingophospholipids. Sphingobacterium species are ubiquitous and isolated from natural environments, such as soil and water. However, they rarely cause infections in humans. Only a limited number of cases have been reported in elderly and immunocompromised patients with underlying diseases and predisposing factors.
Case presentation
An 80-year-old Japanese man with chronic obstructive pulmonary disease and congestive heart failure visited the Kariya Toyota General Hospital, Aichi, Japan with the chief complaint of fever accompanied by chills and left leg pain. At initial presentation, he was distressed and dyspneic. He was febrile (38.8 °C), and his left foot was swollen with reddening and tenderness. We diagnosed him as having cellulitis, and he was hospitalized for antibiotic therapy. Initially, he was treated with intravenously administered cefazolin, but after the isolation of a glucose non-fermenting Gram-negative rod from blood cultures, we decided to switch cefazolin to intravenously administered meropenem on day 4, considering the antibiotic resistance of the causative organism. The causative organism was identified as S. spiritivorum on day 6. His condition gradually stabilized after admission. Meropenem was switched to orally administered levofloxacin on day 12. He was discharged on day 16 and treated successfully without any complications.
Conclusions
Although S. spiritivorum is rare, with limited cases isolated from cellulitis, it should be considered as a causative organism in elderly and immunocompromised patients with cellulitis. Blood cultures are the key to correct diagnosis and appropriate treatment.
Background
Sphingobacterium spiritivorum (S. spiritivorum) is a glucose non-fermenting Gram-negative rod (GNF-GNR), formerly classified as one of the Flavobacterium species [1]. It is characterized by a large number of cellular membrane sphingophospholipids [1]. Sphingobacterium species are ubiquitous and isolated from natural environments, such as soil and water. However, they rarely cause infection in humans. Only a limited number of cases have been reported in elderly and immunocompromised patients with underlying disease and predisposing factors [2,3,4,5,6]. However, S. spiritivorum has the potential of causing fatal infections and bacteremia, particularly in elderly and immunocompromised patients. Although our case is not the first case report of S. spiritivorum infection isolated from humans, we propose that it is important to consider S. spiritivorum as a causative organism in selected patients with cellulitis.
Case presentation
An 80-year-old Japanese man presented to our hospital with complaints of fever and left leg pain, as well as bilateral lower extremity swelling. Although mild edema was always observed in his bilateral lower extremities, it gradually worsened 1 week prior to admission. On the day of admission, he had high fever accompanied by chills. He denied any recent leg trauma. His past medical history was significant for pulmonary tuberculosis at 30 years of age, chronic obstructive pulmonary disease (COPD), and congestive heart failure (CHF). A pacemaker was inserted because of atrial fibrillation (AF) with symptomatic bradycardia. He was an ex-tobacco smoker (100 pack year history) and did not drink alcohol. His maintenance medications were dabigatran (220 mg), furosemide (20 mg), and an inhaled corticosteroid/long-acting β2-agonist.
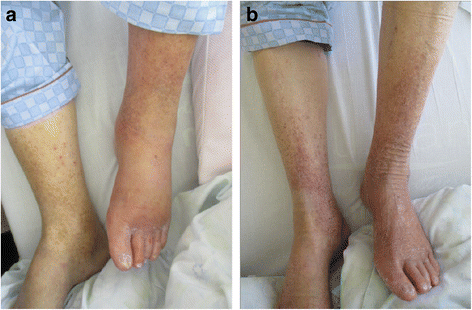
At initial presentation, he was alert and oriented but appeared distressed. His vital signs were as follows: body temperature, 38.8 °C; blood pressure, 135/90 mmHg; heart rate, 96 beats per minute with irregular rhythm; blood oxygen saturation, 93% with room air; and respiratory rate, 22 breaths per minute. He had a barrel-shaped chest, coarse crackles were heard over the lung base, and wheezes were heard over both lung fields. Pitting edema was observed in his lower extremities. His left foot had more erythema and edema than his right foot (Fig. 1). His left lower extremity was warm and tender to touch. There were no skin breaks or other potential infection entry sites. Tinea pedis was ascertained by a potassium hydroxide test.
Appearance of lower extremities of the patient on the day of admission (a) and after treatment (b). On the day of admission, reddening and swelling were observed on the left leg. Dermatophyte was positive in the toe webs as per a potassium hydroxide test
Arterial blood gas analysis showed the following results: pH, 7.408; partial pressure of carbon dioxide, 44 mmHg; partial pressure of oxygen, 72 mmHg; bicarbonate, 22.5 mmol/L; and lactate, 1.8 mmol/L. A complete blood count revealed the following results: white blood cells, 9,000/μL; red blood cells, 384 × 10 4 /μL; hemoglobin, 12.4 g/dL; and platelets, 9.6 × 10 4 /μL. Chemistry results were as follows: serum creatinine, 0.81 mg/dL; blood urea nitrogen, 19.0 mg/dL; albumin, 3.7 g/dL; total bilirubin, 2.1 mg/dL; aspartate aminotransferase, 43 U/L; alanine aminotransferase, 22 U/L; C-reactive protein, 0.36 mg/dl; and brain natriuretic peptide (BNP), 471 pg/mL (our patient’s basal BNP level was approximately 100 pg/mL). A coagulation test showed prolonged prothrombin time-international normalized ratio (1.29) and activated partial thromboplastin time (52.3 seconds). A chest X-ray showed a nodular lesion on the right pulmonary apex compatible with previous tuberculous infection without any infiltrations. An electrocardiogram showed AF with pacemaker rhythm without any sensing and pacing failures. Based on these results, we diagnosed our patient as having cellulitis and immediately admitted him to hospital because his respiratory status continued to worsen, necessitating supplemental oxygen therapy for dyspnea relief. We also considered a risk of sepsis and mortality because his sequential organ failure assessment score was 5 points (2 points greater than baseline) at initial presentation [7].
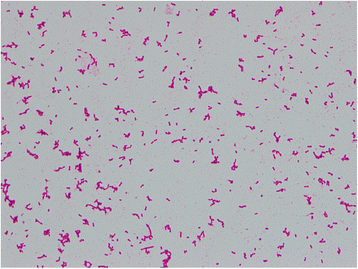
Cefazolin (1 g every 8 hours) was initially administered intravenously to treat his cellulitis, but after 25 hours of incubation, two sets of aerobic blood culture bottles (BD BACTEC™ Plus Aerobic/F Medium; BD Diagnostics, Sparks, MD, USA) were found to be positive (detected by BD BACTEC™ FX, Blood Culture System; BD Diagnostics, Sparks, MD, USA) for GNRs (Fig. 2). The positive culture broth was inoculated onto a blood agar plate (BD BBL™ Trypticase™ Soy Agar with 5% Sheep Blood; Nippon Becton Dickinson Company, Fukushima, Japan) and light yellow colonies were observed after incubation of 24 hours at 37 °C. The causative organism was confirmed as GNF-GNR on day 4. Accordingly, we switched antibiotics to intravenously administered meropenem (1 g every 8 hours) on the same day, considering antibiotic resistance. On day 6, the causative organism was identified as S. spiritivorum. It was identified by BD PHOENIX™ System (BD Diagnostics, Sparks, MD, USA) and matrix-assisted laser desorption/ionization time of flight mass spectrometry, using Microflex LT with MALDI Biotyper version 3.1 database (Bruker Daltonik, Bremen, Germany). Our patient’s condition gradually improved with the antibiotic use. We decided to switch antibiotics to orally administered levofloxacin (500 mg/day) on day 12, considering the antibiotic sensitivity of S. spiritivorum isolated from the blood culture (Table 1). Trimethoprim/sulfamethoxazole was an alternative but was not used out of concern for adverse drug reactions considering our patient’s age. He was discharged on day 16 without any complications, and the antibiotic was discontinued on the same day. We followed up with him 2 weeks after discharge, during which he did not have any residual symptoms related to cellulitis.
Gram stain of the organism isolated from blood culture (magnification, ×1000). Gram-negative short rods were seen
Discussion
Sphingobacterium species are aerobic, Gram-negative, short rod, non-motile, non-spore-forming bacteria. They are oxidase-positive, catalase-positive, and urease-positive and indole-negative and produce light yellow colonies on blood agar plates [1]. Thus far, more than 20 species in the genus Sphingobacterium have been reported based on 16S ribosomal ribonucleic acid gene sequencing [8] and the number of isolated species is increasing. S. spiritivorum was first isolated from a human clinical specimen by Holmes et al. in 1982 [9] and was initially described as Flavobacterium spiritivorum. In 1983, Yabuuchi et al. first proposed Sphingobacterium as a new genus [10]. The genus Sphingobacterium differs from the genus Flavobacterium by high cellular membrane concentrations of sphingophospholipid and ceramide. Naka et al. performed a structural analysis of sphingophospholipids in S. spiritivorum, thereby purifying a novel sphingolipid among eukaryotic and prokaryotic cells [11].
Sphingobacterium species are ubiquitous and commonly isolated from soil, plants, and water, but rarely from human infection sites. Sphingobacterium multivorum and S. spiritivorum were isolated from very few existing cases. Lambiase et al. reported the isolation of S. multivorum and S. spiritivorum from the sputum of patients with cystic fibrosis [12]. Recently, the first human case of Sphingobacterium hotanense infection in an elderly patient was reported [13]. In that case, scratches on the right arm caused by a rooster were the suspected infection entry site from soil.
Sphingobacterium species are resistant to commonly used antibiotics [1]. S. multivorum can produce an extended-spectrum β-lactamase and a metallo-β-lactamase, which make it resistant to third-generation cephalosporins and carbapenems, respectively [14]. S. spiritivorum is susceptible to carbapenems. Quinolones, trimethoprim-sulfamethoxazole, and ceftazidime are effective in vitro, which is compatible with previous clinical reports [12]. S. spiritivorum isolated from the present case was susceptible to the antibiotics listed above. In the present case, we observed a good clinical course with intravenously administered meropenem followed by orally administered levofloxacin.
We identified five previously reported cases of S. spiritivorum infection in the English literature [2,3,4,5,6] (Table 2). Three cases were caused by cellulitis [2, 3, 6] and two cases by catheter-related blood stream infection [4, 5]. In most of these cases, the patients had predisposing factors and underlying diseases, such as Parkinson’s disease (with chronic venous stasis due to akinesia and injuries from frequent falls, which are risk factors for cellulitis) [2, 3], refractory anemia [4], acute myeloid leukemia treated with chemotherapy [5], and end-stage renal disease on hemodialysis [6]. One case of extrinsic allergic alveolitis (hypersensitivity pneumonitis) caused by S. spiritivorum [15] was not included because it was not a direct infection but was caused by a hypersensitivity reaction against organism-derived allergens [16]. In our case, edema due to CHF was a risk factor for cellulitis [17]. Aging and COPD can also increase susceptibility to infections [18, 19]. Tinea pedis is a risk factor for cellulitis [20] because it may provide entry sites for infections [21] and changes in bacterial flora [22].
Although obtaining blood cultures of patients with cellulitis may not be cost effective, given the low rate of positive blood cultures (2.0%) [23], we could not have made a correct diagnosis in the present case without blood cultures. Mills and Chen reviewed several studies and concluded that obtaining blood cultures does not significantly alter treatment or aid in diagnosing the causative organism in immunocompetent patients with acute cellulitis [24]. In addition, the current Infectious Diseases Society of America (IDSA) guidelines do not recommend routine performance of blood cultures in patients with cellulitis; however, performing blood cultures is recommended in patients with malignancy, chemotherapy, neutropenia, severe cell-mediated immunodeficiency, immersion injuries, and animal bites [25]. Peralta et al. reported the absence of previous antibiotic treatment and the presence of two or more comorbid factors including obesity, COPD, diabetes, alcohol addiction, liver cirrhosis, CHF, and immunocompromised condition were associated with bacteremia in patients with cellulitis [26]. Lee et al. proposed an initial diagnostic prediction model with four independent predictors for estimating probability of bacteremia in patients with cellulitis: age ≥ 65 years, involvement of non-lower extremities, liver cirrhosis, and systemic inflammatory response syndrome [27]. In a recent study, van Daalen et al. reported the blood culture positivity rate was higher than the rates reported by IDSA guidelines in hospitalized patients with skin and soft tissue infections, particularly in patients with severe comorbidity [28]. Evaluation of patients’ comorbidity is critical to making decisions to perform blood cultures in patients with cellulitis. Considering S. spiritivorum was isolated from blood cultures in all of the previous reports, performing blood cultures in patients with cellulitis with comorbid risk factors can be useful to identify the causative organism and important for appropriate treatment.
Conclusions
S. spiritivorum is a rare causative organism of cellulitis, with a limited number of reported cases in the literature. In the present case, aging and COPD could have been the risk factors for infection, and edema due to CHF was a predisposing factor for cellulitis. Tinea pedis could have produced an infection entry site. Although our patient was initially septic, he was successfully treated by administration of targeted antibiotics. Blood cultures were key to identifying the causative organism in the present case. We should consider S. spiritivorum as a potential causative organism of cellulitis, particularly in patients with comorbid risk factors.